 Clinical Thoughts for the week
Clinical Thoughts for the week
- G-tubes can be a bridge to becoming a healthy oral eater. (not a failure)
- It takes a village to help children and parents with these complicated feeding issues.
- When you help a child learn to be a successful eater- you change a family’s life.
- If progress is to be made, it is essential for caregivers and parents to follow through with feeding plan at home and be an active part of the process in feeding therapy. Feeding skill improvement is dependent on successful practice over time.
- Don’t underestimate the benefit of helping a child’s gut feel better with medical and nutritional management.
- Don’t underestimate the benefits of proper nutrition and growth and the positive effects it can have on a child’s energy level, demeanor, and gross motor skills. (and for feeding therapists don’t assume someone else is looking at this the same way we would!)
Case:
Case: weight for age:
 Let me tell you about MK. We discharged a child this week, a 10 year old who we were able to take from not eating and failure to thrive to “eating everything” in 3 years with the help of a g-tube and intensive feeding program.
Let me tell you about MK. We discharged a child this week, a 10 year old who we were able to take from not eating and failure to thrive to “eating everything” in 3 years with the help of a g-tube and intensive feeding program.
case: Length for age
 MK presented with: failure to thrive, GI problems (abdominal pain, constipation, vomiting, gagging), aversive feeding behavior (refusal, avoidance, behaviors, very limited diet, inconsistent eating, skipping meals, ADHD, behavioral difficulties outside eating.
MK presented with: failure to thrive, GI problems (abdominal pain, constipation, vomiting, gagging), aversive feeding behavior (refusal, avoidance, behaviors, very limited diet, inconsistent eating, skipping meals, ADHD, behavioral difficulties outside eating.
case: BMI
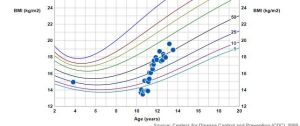 She had struggled with feeding difficulties and poor weight gain since birth so her family had been dealing with this for 10 years!
She had struggled with feeding difficulties and poor weight gain since birth so her family had been dealing with this for 10 years!
MK’s food diet consisted of chicken nuggets only from McDonald’s, fruit loops, sometimes with milk, smoked pork chops that are of specific brand, French fries seasoned from Walmart, Lays pack potato chips, Pringles, Fritos, Doritos, Cheetos, shredded cheese, crackers and Ensure that he may refuse. She does not eat other meats, fruits or vegetables.
She was isolated at school because of her eating and ate with a teacher instead of her peers which was too distracting. She needed a high calorie supplement drink because of her poor growth and refusal to eat. Parents were worried, stressed, fatigued, and burned out with the feeding issue. MK had “failed” traditional feeding therapy and they did not know what to do.
Team approach:
The first 6 months: We started MK’s care with medical and nutritional management which involved GI treated reflux, constipation, and gut pain. Multiple tests were done and labs were drawn. Nutrition worked with the family on meeting caloric needs with supplements that were tolerated on her GI tract as well as vitamins and food choices. Therapy worked on strategies to increase acceptance of a variety of foods and increase volume. Therapy worked on increasing what MK would eat and she would try almost anything in therapy but would not at home.
At the 6 months mark- weight gain, growth, and feeding was inconsistent and transition to home was difficult because of MK’s severe aversive behaviors. At that point, due to MK’s poor weight gain, a G-tube was recommended to the family. This is never an easy decision but MK’s poor nutritional status was effecting her health. G-tube was placed which allowed us to provide better nutrition while keeping MK comfortable.
Our team also made the recommendation to refer MK to an intensive feeding program. Some children need the intensity of daily therapy to improve. Again parents agreed, and MK completed a 4 week intensive feeding program at St Joseph’s pediatric feeding program in Paterson, NJ (www.feedingcenter.org). She left the program with increased variety of foods accepted but still struggled with volume.
1 – 2 1/2 years: She came back to out -patient therapy ( 1-2 sessions per months with decreasing frequency as she improved) and good weight gain (with the g-tube).
After completing the intensive program, there was a plan in place for 15 bites of 3 different solid foods. It often took 1 hour to get these 15 bites in due to MK’s refusal and distraction behaviors. A behavioral program was utilized with rewards in place for timely acceptance. Caregivers practiced at home when MK was not in school. Slow progress was made. MK was able to increase her volume of foods and liquids, increase her variety, gain weight, and improve with oral -motor stamina for chewing solid foods.
As her oral eating improved and MK’s weight increased, her g-tube feeds and medicines were adjusted. MK used her feeding tube for 2 years moving from 100% dependence to 100% oral feeding. It was removed 2 ½ years after she received it. Her last meal in therapy was grilled chicken, mashed potatoes, and broccoli which she self fed.
2-3 years: We discharged MK 3 years after meeting her. She is now a successful oral feeder who enjoys food, eats the family meal, eats with her peers at school, eats foods from all food groups, and has proven she can gain weight. Her demeanor is happy and she is energetic and verbally expressed that she now likes to eat. Parent’s feel they have their life back and no longer prepare separate meals, argue about taking bites, or stress about MK’s weight. In fact, at the last visit, they said she wants to eat all the time now.

Just stumbled on this blog. Didn’t even know it existed. Thanks for this story. It gives me hope.
This brought tears to my eyes. What an amazing journey for everyone! It also makes me feel better about our field. I have to admit I’m so disappointed in what so many professionals consider feeding therapy. Congrats!!!